Orchiectomy Surgery in India |
 |
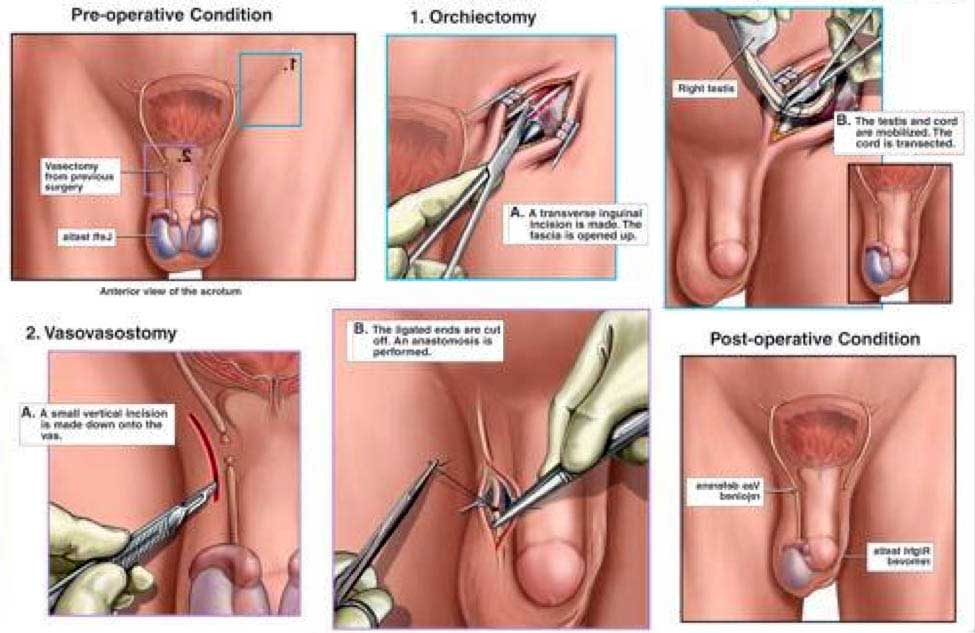
Orchiectomy is the surgical removal of one or both testicles, or testes, in the human male. It is also called an orchiectomy. The removal of both testicles is known as a bilateral orchiectomy, or castration, because the person is no longer able to reproduce. Emasculation is another word that is sometimes used for castration of a male. Castration in women is the surgical removal of both ovaries (bilateral oophorectomy)
Purpose
An orchiectomy is done to treat cancer or, for other reasons, to lower the level of testosterone, the primary male sex hormone, in the body. Surgical removal of a testicle is the usual treatment if a tumor is found within the gland itself, but an orchiectomy may also be performed to treat prostate cancer or cancer of the male breast, as testosterone causes these cancers to grow and metastasize (spread to other parts of the body). An orchiectomy is sometimes done to prevent cancer when an undescended testicle is found in a patient who is beyond the age of puberty.
A bilateral orchiectomy is commonly performed as one stage in male-to-female (MTF) gender reassignment surgery. It is done both to lower the levels of male hormones in the patient's body and to prepare the genital area for later operations to construct a vagina and external female genitalia.
Reasons for Procedure
An orchiectomy may be done to treat:
-
Prostate cancer that has spread
-
Testicular cancer
-
Testicular torsion (when twisting of the spermatic cord cuts off blood supply)
It can also be a diagnostic procedure to determine if cancer is present when a mass is found during ultrasound.
Description
You will be prepared for surgery. The genital area will be shaved and sterilized. An IV will be placed in your arm for medicines and fluids.
Once you are asleep, the doctor will make a small incision in the groin area or in the scrotum. The testicle is pulled up from the scrotal sac. The cord that connects the testicle to the scrotum is clamped and sutured. The testicle is removed. Absorbable stitches will be used to close all incision areas.
A prosthetic testicle is sometimes placed into the scrotum. This can be done at the time of the surgery or at a later date.
There are three basic types of orchiectomy: simple, subcapsular, and inguinal (or radical). The first two types are usually done under local or epidural anesthesia, and take about 30 minutes to perform. An inguinal orchiectomy is sometimes done under general anesthesia, and takes between 30 minutes and an hour to complete.
Simple orchiectomy
A subcapsular orchiectomy is also performed for treatment of prostate cancer. The operation is similar to a simple orchiectomy, with the exception that the glandular tissue is removed from the lining of each testicle rather than the entire gland being removed. This type of orchiectomy is done primarily to keep the appearance of a normal scrotum.
Subcapsular orchiectomy
A subcapsular orchiectomy is also performed for treatment of prostate cancer. The operation is similar to a simple orchiectomy, with the exception that the glandular tissue is removed from the lining of each testicle rather than the entire gland being removed. This type of orchiectomy is done primarily to keep the appearance of a normal scrotum.
Inguinal orchiectomy
An inguinal orchiectomy, which is sometimes called a radical orchiectomy, is done when testicular cancer is suspected. It may be either unilateral, involving only one testicle, or bilateral. This procedure is called an inguinal orchiectomy because the surgeon makes the incision, which is about 3 in (7.6 cm) long, in the patient's groin area rather than directly into the scrotum. It is called a radical orchiectomy because the surgeon removes the entire spermatic cord as well as the testicle itself. The reason for this complete removal is that testicular cancers frequently spread from the spermatic cord into the lymph nodes near the kidneys. A long non-absorbable suture is left in the stump of the spermatic cord in case later surgery is necessary.
After the cord and testicle have been removed, the surgeon washes the area with saline solution and closes the various layers of tissues and skin with various types of sutures. The wound is then covered with sterile gauze and bandaged.
Diagnosis
The doctor may suspect that a patient has prostate cancer from feeling a mass in the prostate in the course of a rectal examination, from the results of a transrectal ultrasound (TRUS), or from elevated levels of prostate-specific antigen (PSA) in the patient's blood. PSA is a tumor marker, or chemical, in the blood that can be used to detect cancer and monitor the results of therapy. A definite diagnosis of prostate cancer, however, requires a tissue biopsy. The tissue sample can usually be obtained with the needle technique. Testicular cancer is suspected when the doctor feels a mass in the patient's scrotum, which may or may not be painful. In order to perform a biopsy for definitive diagnosis, however, the doctor must remove the affected testicle by radical orchiectomy.
Preparation
-
All patients preparing for an orchiectomy will have standard blood and urine tests before the procedure. They are asked to discontinue aspirin-based medications for a week before surgery and all non-steroidal anti-inflammatory drugs (NSAIDs) two days before the procedure. Patients should not eat or drink anything for the eight hours before the scheduled time of surgery.
-
Most surgeons ask patients to shower or bathe on the morning of surgery using a special antibacterial soap. They should take extra time to lather, scrub, and rinse their genitals and groin area.
-
Patients who are anxious or nervous before the procedure are usually given a sedative to help them relax.
-
Cancer. Patients who are having an orchiectomy as treatment for testicular cancer should consider banking sperm if they plan to have children following surgery. Although it is possible to father a child if only one testicle is removed, some surgeons recommend banking sperm as a precaution in case the other testicle should develop a tumor at a later date.
-
Gender reassignment. Most males who have requested an orchiectomy as part of male-to-female gender reassignment have been taking hormones for a period of several months to several years prior to surgery, and have had some real-life experience dressing and functioning as women. The surgery is not performed as an immediate response to the patient's request.
-
Because the standards of care for gender reassignment require a psychiatric diagnosis as well as a physical examination , the surgeon who is performing the orchiectomy should receive two letters of evaluation and recommendation by mental health professionals, preferably one from a psychiatrist and one from a clinical psychologist.
Aftercare
Patients who are having an orchiectomy in an ambulatory surgery center or other outpatient facility must have a friend or family member to drive them home after the procedure. Most patients can go to work the following day, although some may need an additional day of rest at home. Even though it is normal for patients to feel nauseated after the anesthetic wears off, they should start eating regularly when they get home. Some pain and swelling is also normal; the doctor will usually prescribe a pain-killing medication to be taken for a few days.
Other recommendations for aftercare include:
-
Drinking extra fluids for the next several days, except for caffeinated and alcoholic beverages.
-
Avoiding sexual activity, heavy lifting, and vigorous exercise until the follow-up appointment with the doctor.
-
Taking a shower rather than a tub bath for a week following surgery to minimize the risk of absorbable stitches dissolving prematurely.
-
Applying an ice pack to the groin area for the first 24–48 hours.
-
Wearing a jock strap or snug briefs to support the scrotum for two weeks after surgery.
Some patients may require psychological counseling following an orchiectomy as part of their long-term aftercare. Many men have very strong feelings about any procedure involving their genitals, and may feel depressed or anxious about their bodies or their relationships after genital surgery. In addition to individual psychotherapy, support groups are often helpful. There are active networks of prostate cancer support groups in Canada and the United States as well as support groups for men's issues in general.
Long-term aftercare for patients with testicular cancer includes frequent checkups in addition to radiation treatment or chemotherapy. Patients with prostate cancer may be given various hormonal therapies or radiation treatment.
Risks
Some of the risks for an orchiectomy done under general anesthesia are the same as for other procedures. They include deep venous thrombosis, heart or breathing problems, bleeding, infection, or reaction to the anesthesia. If the patient is having epidural anesthesia, the risks include bleeding into the spinal canal, nerve damage, or a spinal headache.
Specific risks associated with an orchiectomy include:
-
Loss of sexual desire (This side effect can be treated with hormone injections or gel preparations.)
-
-
Hot flashes similar to those in menopausal women, controllable by medication
-
Weight gain of 10–15 lb (4.5–6.8 kg)
-
Mood swings or depression
-
Enlargement and tenderness in the breasts
-
Fatigue
-
Loss of sensation in the groin or the genitals
-
Osteoporosis (Men who are taking hormone treatments for prostate cancer are at greater risk of osteoporosis.)
-
An additional risk specific to cancer patients is recurrence of the cancer.
-
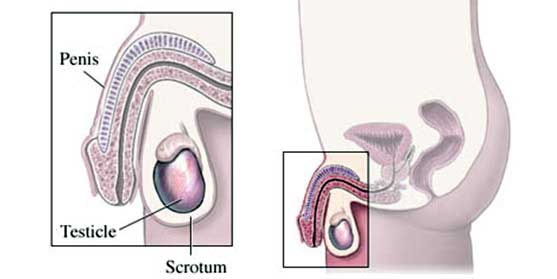
Orchiectomy is a surgery to remove one or both testicles.
Male Genitalia
Call Your Doctor
After arriving home, contact your doctor if any of the following occurs:
-
Increasing pain, discharge, redness, or swelling at the incision site
-
Pus or odor from the incision site
-
A lot of bleeding
-
Stitches loosen or fall out
-
Signs of infection, including fever and chills
|
 |
|
|
|
