Prostate Cancer Treatment in India – Overview, Causes, Symptoms and Cost |
 |
Prostate Cancer, (PCa), is the most common cancer in men in the US today. In 1997 there were 240,000 newly discovered cases and about 40,000 deaths. These numbers have started to drop as the result of the development of a screening test, PSA, and much improved public awareness of the importance of seeking evaluation on a regular schedule.
Prostate Cancer is much more common in the developed world, especially in western Europe and the Americas. The causes are unknown but are probably related to lifestyle and dietary factors. Heredity and race play roles in causation as there are families with a high incidence of prostate cancer, and it is much more frequently found in African Americans than Caucasians. The disease is rare in Africa and Asia, but occurs more frequently in later immigrant generations.
The disease is rare before age 40. The incidence rises with age, and by age 80, 70+% of men will have prostate cancer, although the aggressiveness of the disease decreases with late age of onset.
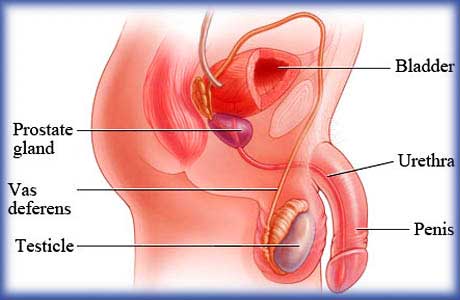
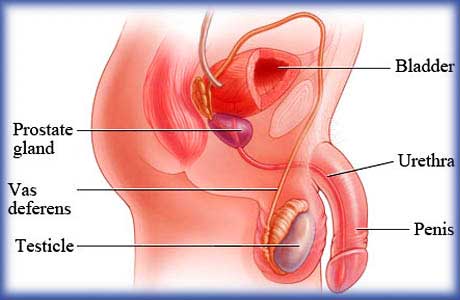
Anatomy and Physiology
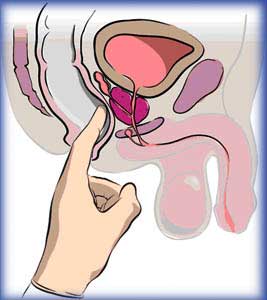
The prostate gland, (very frequently mispronounced prostRate), lies deep in the pelvis. It surrounds the urethra, the urine tube running from the bladder, through the prostate and the penis. It is just in front of the rectum so that part of the gland may be easily examined by a simple Digital Rectal Examination, (DRE). In young men it is usually the size of a walnut, but may grow with age to the size of a lemon, or even larger. It supports the ejaculatory ducts, or sperm tubes, but appears not to have any other function in humans.
Symptoms
Prostate cancer usually exists without symptoms!!! Some patients may have symptoms of having to urinate frequently or slowly, or have urinary burning or blockage or bleeding. These symptoms usually come from other conditions such as infection or inflammation or overgrowth, but may be associated with prostate cancer. When these symptoms occur the patient should seek urologic evaluation. When the cancer has spread, bone pain is a common symptom.
Who Should be Examined for Prostate Cancer?
All men over 50 and below 80 should have an annual prostate cancer examination. All men over 40 with strong family histories, (fathers, brothers or any two close relatives), and all African-American men over 40 should have an annual exam. In those few families with multiple males having had prostate cancer screening might be considered at an earlier age.
Prostate cancer is very common in men over 80, but is usually a slow growing, non life threatening disease. Men over 80 should have an annual DRE for prostate and colorectal examination, and if the prostate is abnormal a PSA may be obtained. (See below under treatment).
The Prostate Examination
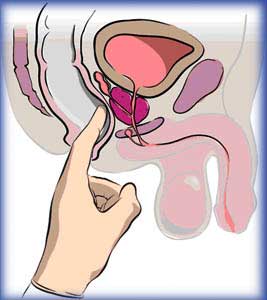 The prostate examination consists of two parts, a digital rectal examination, (DRE), and a blood test, the PSA or, prostate specific antigen. The combination of the two examinations significantly increases the detection of prostate cancer over either test alone. The prostate examination consists of two parts, a digital rectal examination, (DRE), and a blood test, the PSA or, prostate specific antigen. The combination of the two examinations significantly increases the detection of prostate cancer over either test alone.
The DRE is performed by the examiner gently inserting a finger into the rectum and palpating the gland for size, shape, consistency, and nodules or lumps. The examiner may also check for colon or rectal cancer or other conditions. Prostate nodules should not be ignored. Although about half of prostate nodules found will not be cancerous, the examiner cannot tell from the examination alone whether cancer is present. Some prostate cancers cannot be felt by DRE because they lie in a click picture to enlarge part of the gland that the finger cannot reach, or they are too small to feel or they just do not feel abnormal. All nodules require further evaluation.
PSA or Prostate Specific Antigen, is a blood test that helps detect prostate cancer. PSA is a fuzzy test and cannot diagnose prostate cancer by itself!. Many other conditions such as prostate infection or inflammation, or urinary tract infection may raise the PSA. A high PSA does not mean cancer is present and a normal PSA does not rule out the presence of prostate cancer The normal values for PSA are 0 to 4. Borderline levels are 4 to 10 and when it is over 10 it is considered high.
Prostatitis may artificially elevate PSA, a a rapid rise in PSA should usually be treated for several weeks with appropriate antibiotics and then repeated .
The use of Proscar or Propecia as well as many of the proprietary "prostate medicines" sold over the counter, which include saw palmetto will artificially lower PSA levels. For patients on any of these drugs, the normal upper limit of PSA is reduced to 2-2.5. Patients using any of these medications should inform their doctors!!
When the PSA levels are between 4 and 10 a second fuzzy blood test, the Total vs. Free PSA ratio may be helpful. While high ratios, over 25%, suggest benign disease, and low ratios, under 15%, suggest cancer, there are many false positive and negative results, and the evaluation of the results are best left to a urologist. This test is not valid for PSA's less than 4 nor greater than 10.
A third indicator is PSA velocity. If the PSA is rising more than 0.7 per year it is considered suspicious and should be taken into the consideration for biopsy
Sometimes when the PSA is borderline or elevated, or a nodule is present, and there are symptoms suggestive of infection or inflammation, the urologist, (this decision is best left to an expert), may decide to treat the condition with antibiotics for 2 to 4 weeks and repeat both the PSA and the examination. If both examinations return to normal, cancer is usually not present, and a repeat examination in 3 to 6 months is indicated.
When to Evaluate for Prostate Cancer
When a prostate nodule has been found on DRE, or the PSA is borderline or elevated, (greater than 4), or the PSA is rising faster than 0.7 per year, consultation with a urologist, should be obtained. The urologist, along with the patient can then plan the further evaluation.
Evaluation of Possible Prostate Cancer
The Consultation
The Urologist will take a History , asking questions about the patient's urinary symptoms, previous evaluations, sexual functioning and general medical history. A physical examination will include at least a careful examination of the genitalia and a DRE. He will then plan what further tests are needed.
Total and Free PSA Ratio
When the PSA is borderline, between 4 and 10, a total and free PSA ratio may be obtained. Like the PSA it is a fuzzy test, revealing the likelihood of cancer being present, but not a definitive answer. It may help define whether further tests may be needed. A low ratio, less than 15% suggests that there is a high possibility of cancer, ha high ratio, over 25% suggests a low possibility. However there may be false positives and false negatives.
Trans Rectal Ultrasound (TRUS)
TRUS is an examination where a finger-like probe is placed in the rectum, and ultrasound pictures are made of the prostate. TRUS is an even more fuzzy test than the PSA. It is very helpful in directing biopsies to areas of high suspicion, but TRUS is non-diagnostic. It may give information about prostate size, shape, and significant local spread of prostate cancer, but it cannot make or deny the diagnosis of prostate cancer. TRUS should never be done as an isolated test, but only when a biopsy is to be done.
Needle Biopsy of the Prostate
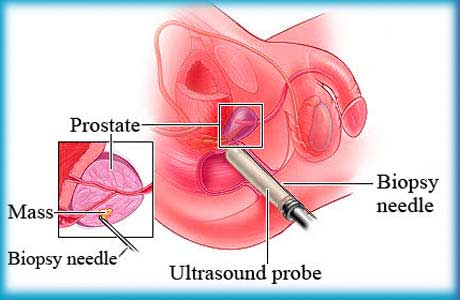 The definitive test to make the diagnosis of prostate cancer is the needle biopsy. A wpe15.gif (33323 bytes) thin needle, guided either by ultrasound or a finger, is inserted through the rectum into the prostate, and a small sample of tissue taken. Usually 6 to 12 samples are taken from nodules, from suspicious areas seen on sonography, or in a pattern sampling the entire prostate. This test has a better than 90% accuracy in diagnosing prostate cancer, although occasional false negative results occur when a small cancer in the gland is not sampled. The test, while uncomfortable is usually done without anesthesia. The definitive test to make the diagnosis of prostate cancer is the needle biopsy. A wpe15.gif (33323 bytes) thin needle, guided either by ultrasound or a finger, is inserted through the rectum into the prostate, and a small sample of tissue taken. Usually 6 to 12 samples are taken from nodules, from suspicious areas seen on sonography, or in a pattern sampling the entire prostate. This test has a better than 90% accuracy in diagnosing prostate cancer, although occasional false negative results occur when a small cancer in the gland is not sampled. The test, while uncomfortable is usually done without anesthesia.
Small amounts of bleeding in the urine, stool or semen are common after biopsy. Significant bleeding, or major infection are occasional complications of needle biopsy, rarely requiring hospitalization.
Preparation includes:
-
Stopping blood thinners, (first check with the doctor who has you on this medication). Aspirin should be stopped at least 5 days before, or if that is contraindicated, a baby aspirin may be taken every other day for several days before.
-
Antibiotics are frequently started the night before the procedure,
-
A cleansing fleet enema should be taken the morning of the test.
-
If you are having sedation you must not eat or drink after midnight the night before. You may take all your medicines with a sip of water.
The biopsy results will usually be available within a week. You should call the office and make an appointment to see the doctor at least one week after the biopsy. We do not give biopsy reports over the phone.
Occasional false negative results are obtained so even if cancer is not found, follow-up appointments MUST be made and kept.
What if the biopsy is positive ?
When prostate cancer has been found, it is not a death sentence! Many patients can be cured of prostate cancer if it has been found early enough, (that's why we look hard and recommend regular examinations and PSA tests). Even if the cancer is not curable many patients can be treated, the cancer slowed down, and they can live for years. Before we can even give a prognosis or plan treatment, the urologist must take into account many factors and perhaps do some more tests. The first factors to evaluate are the Grade and Stage of the cancer.
PIN or Prostate Intraepithelial Neoplasia
PIN is a non cancerous cell abnormality that is frequently associated with prostate cancer. It requires careful evaluation.
Atypia
Sometimes atypical cells are found. These abnormal cells are usually too few in number, or are not "bad" enough to be diagnosed as cancer. They are followed in a similar fashion to PIN
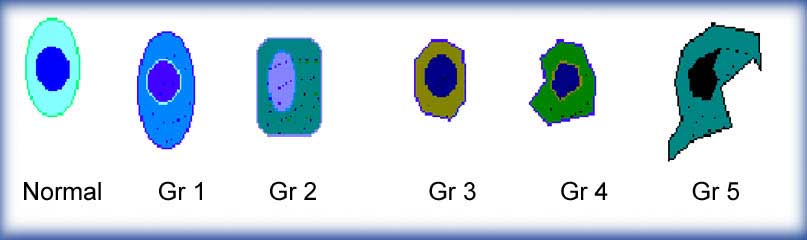
Grade or Gleason Grade
When the pathologist looks at the biopsy he grades the cancer by comparing the appearance of the cancer cells to the appearance of normal prostate tissue. The grades go from Grade 1, almost normal, to Grade 5, very abnormal.
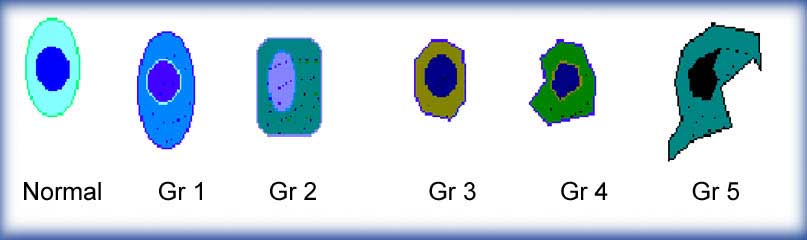
The Pathologist then adds the results from the two greatest areas of cancer and gives a report, for example, (3+2=5). Therefore positive biopsies run from Gleason grade 2, which has a relatively good prognosis, to Gleason grade 10, which does not. The vast majority of biopsies are Gleason grade 6, or moderate.
The Stage of a cancer refers to how far it has progressed. There are several different staging systems but the most commonly used is A, B, C, D. Within each stage there are sub- stages:
Stage A describes a cancer that is only found by elevated PSA and biopsy, or at click to enlargesurgery for obstruction. It is not palpable on DRE. It is localized to the prostate. This type of cancer is usually curable, especially if it is a relatively low Gleason grade.
Stage B Cancer refers to a cancer that can be felt on rectal examination and is click to enlargelimited to the prostate. Other tests, such as bone scans or CT/MRI scans, may be needed to determine this stage, especially if the PSA is significantly elevated or the Gleason grade is 7 or greater. Many Stage B prostate cancers are curable.
Stage C Cancer has already spread beyond the capsule of the prostate into localclick to enlarge organs or tissues, but has not yet metastasized or jumped to other sites. This stage is determined by Digital Rectal Exam, or CT/ MRI scans, and/or Sonography. The bone scan, and , if done, the Prostascint scan are negative. Some Stage C cancers are curable.
Stage D Cancer has already spread, usually to distant lymph nodes, bones or other click to enlarge sites. This is usually determined by bone scan, Prostascint scan or other studies. Stage D cancer is not curable but is treatable
Risk Status
There has been discussion recently about a slightly different classification for planning of therapy of apparently confined prostate cancers: Low, intermediate or high risk.
-
Low Risk comprises those prostate cancer that are low in volume, Stage A or B1/B2, with a Gleason Grade of 6 or less, and a PSA less than 11.
-
Intermediate Risk requires Stage B3 or Gleason Grade 7 or PSA greater than 10.
-
High Risk includes those cancers Gleason grade 7 or above and PSA greater than 10
The choice of what type of therapy is appropriate for a patient with Prostate Cancer: radical prostatectomy, radiation, seeds, combined therapy, observation, cryotherapy or hormonal therapy, is dependant on many factors including: the Gleason Grade and the Stage of the cancer; the patient's age; the patients medical condition; and the patient's desires. There is no absolutely right or wrong way to treat every patient, and what is appropriate for one patient may not be so for another.
In general prostate cancer tends to be less aggressive with increasing age of onset. Indeed, prostate cancer discovered when the patient is over 80 years of age tends to be slow growing, and is usually observed or watched, and treated only if the cancer seems to be growing aggressively. Similarly, patients with other severe medical conditions who are discovered to have prostate cancer may be best observed, and treated only if the prostate cancer is aggressive. Some patients with lower grade, (Gleason 2 - 5) and or very small amounts of cancer found in the gland may elect observation. The risk of developing metastases and incurable disease must be balanced against the desire to avoid treatment.
Younger, healthy prostate cancer patients with curable disease, Stage A, Stage B, and some early Stage C, should be treated aggressively with either surgery, or varied forms of radiation, such as conformal external beam, seed implantation, (brachytherapy), or combined therapy, or possibly with cryotherapy. Classic thinking has been that over the long run, surgery provides a slightly better chance for cure, and should be favored in younger healthier patients. However recent data suggests no great difference between surgery or radiation up to 12 Years. In some cases where there is a high suspicion of local spread: Stage C, or Gleason grade 7 or 8, or a PSA over 10, surgery followed by radiation or combined brachytherapy and external beam irradiation with or without hormone therapy may be indicated.
Patients age 70 to 79 or patients with other serious, life threatening diseases, should be treated with one of the forms of radiation therapy, cryotherapy, or in some cases, observation
Sometimes, neoadjuvant, short term hormonal treatment, used in combination with radiation treatments is appropriate.
Historically Prostate cancer patients with advanced cancer: Stage D, or extensive Stage C, disease were best treated with hormonal therapy. While not curing prostate cancer, hormonal therapy frequently slows its course and prolongs life and comfort. However, recent research suggests that aggressive treatment of the local cancer, with surgery or combined: hormone therapy, external beam irradiation and seeds, PLUS long term hormonal suppression significantly increases life expectancy and cancer free survival. This is a major change in therapy.
Patients with Gleason grade 8, 9 or 10 have high risk cancer. Treatment is controversial. Historically, aggressive treatment was not offered, however recent studies suggest that early aggressive treatment with combinations of surgery or radiation along with long term early hormonal therapy, with or without taxane based chemotherapy may increase survival or disease free periods in these cases.
There is no one "right" way to treat any one patient, and a discussion with the urologist, is necessary to arrive at an appropriate treatment plan.
Late stage prostate cancer
Refers to Stage D prostate cancer that has spread widely, and is becoming or has become Hormone Resistant (HRPC) or unresponsive to standard hormone therapy.
Sometimes cycling antiandrogen therapy may induce one or several more remissions. This involves stopping the antiandrogen and following the PSA. If a significant drop occurs the drug is excluded until the PSA rises to similar levels, and the it is reintroduced. In some patients several such cycles may occur. Alternatively, changing the LHRH medication may induce a short response. Checking testosterone levels be helpful as some patients do not respond well to LHRH or escape response. If the testosterone level remains high, surgical removal of the testicles, (orchiectomy) may be helpful. Sometimes high dose Casodex (150 mg/day) may block the high testosterone levels. (This dose is NOT FDA approved yet!!)
Chemotherapy has in general not had excellent results in late stage prostate cancer, but searches for an active combination continues. Occasional patients respond well. Ketokonazole or Mitoxantrone and prednisone hahave shown some promise in slowing down the disease and/or relieving pain in patients with painful bony metastases. Trials with taxotere or tamoxiphen sometimes combined with estramustine or prednisone have also shown responses in a significant number of patients. Thalidomide is also under study. There are many clinical trials with other drugs being carried out at many centers including ours. An older regimen using DES or estrogens is being revisited, and some patients have had good responses, but there is a risk of cardiovascular complications
For patients who have bony metastases several different treatments such as external beam radiotherapy, Strontium 89, Samarium153, or bisphosphonates may be very helpful. A new bisphosphonate, Zometa, can delay bony complications of prostate cancer when administered at the earliest signs of bony metastases, or when the cancer becomes hormone resistant.
External beam radiotherapy may be given to specific body areas, especially bones that are involved with prostate cancer and are painful, or are in danger of breaking.
Bisphosphonates which act on the rapidly growing bone in metastases are being used to control pain, the newer more potent bisphosphonates may also reduce and delay skeletal complications of metastatic PCa.. Bisphosphonates may also be used to prevent the osteoporosis of long term hormone therapy.
Radioactive Samarium 153 (Quadramet) Is an intravenously administered medication that is picked up by the rapidly growing prostate cancer cells in bony metastases. It radiates those cells, killing many of them, and providing relief of pain in many patients. It has the advantage over Strontium89 in that several repeated courses may be given in many patients.
Radioactive Strontium 89 is a similar drug to Samarium 153, but frequently only a single course can be given due to bone marrow effects.
Immunotherapy, Dendritic cell therapy and Monoclonal antibodies are research tools being used in select centers.
Related Links:
|
 |
|
|
|




 The prostate examination consists of two parts, a digital rectal examination, (DRE), and a blood test, the PSA or, prostate specific antigen. The combination of the two examinations significantly increases the detection of prostate cancer over either test alone.
The prostate examination consists of two parts, a digital rectal examination, (DRE), and a blood test, the PSA or, prostate specific antigen. The combination of the two examinations significantly increases the detection of prostate cancer over either test alone.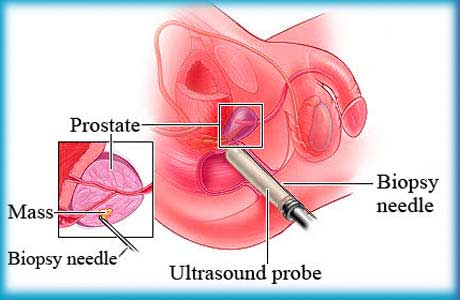 The definitive test to make the diagnosis of prostate cancer is the needle biopsy. A wpe15.gif (33323 bytes) thin needle, guided either by ultrasound or a finger, is inserted through the rectum into the prostate, and a small sample of tissue taken. Usually 6 to 12 samples are taken from nodules, from suspicious areas seen on sonography, or in a pattern sampling the entire prostate. This test has a better than 90% accuracy in diagnosing prostate cancer, although occasional false negative results occur when a small cancer in the gland is not sampled. The test, while uncomfortable is usually done without anesthesia.
The definitive test to make the diagnosis of prostate cancer is the needle biopsy. A wpe15.gif (33323 bytes) thin needle, guided either by ultrasound or a finger, is inserted through the rectum into the prostate, and a small sample of tissue taken. Usually 6 to 12 samples are taken from nodules, from suspicious areas seen on sonography, or in a pattern sampling the entire prostate. This test has a better than 90% accuracy in diagnosing prostate cancer, although occasional false negative results occur when a small cancer in the gland is not sampled. The test, while uncomfortable is usually done without anesthesia.